- When to have reconstruction
- Additional surgeries
- What type of reconstruction is best for me?
- Implant reconstruction
- Autologous/autogenous reconstruction (reconstruction procedures that use your own tissue)
- Comparing reconstruction methods
- Other procedures
- Oncoplastic surgery
- Bilateral therapeutic mammoplasty
- Watch: Considering reconstruction after breast cancer
Breast reconstruction surgery aims to rebuild the shape of the breast following a mastectomy or partial mastectomy.
The aim of this procedure is to restore a balanced and normal look in your bra and clothes; however the resulting breast "mound" usually has no nipple and it's not possible for the surgeon to restore sensation to your breast.
In many (but not all) cases a new nipple can be created surgically once the breast has healed and an areola can be tattooed in place.
In some cases the original nipple may be conserved.
Video
Webinar: A Tale of Two Reconstructions
Choosing what’s right for your reconstruction can be difficult, especially with the overwhelming choices, from implants to tissue transplants and immediate to delayed. Our webinar can help you figure out what’s best for you!
When to have reconstruction
Most women who opt for breast reconstruction have it done at the same time as the initial surgery. This is known as immediate reconstruction. You will be referred to a plastic surgeon or oncoplastic breast surgeon as part of the surgical planning process. However, there are often valid reasons why a delayed reconstruction is recommended:
- There is an urgent need for chemotherapy. If chemotherapy treatment needs to be undertaken first, it's important to talk with your surgeon about wanting reconstruction once this has been completed.
- Post-mastectomy radiation will be required. (Radiation treatment can have an adverse effect on cosmetic outcomes of some reconstructions, particularly implants.) Flap reconstruction, using your own tissue, has better outcomes after radiation treatment.
- Factors such as smoking, diabetes and obesity increase the risk of infection, poor wound healing and other complications and reconstruction may have to be delayed until these risks have been lowered.
Some women may prefer to have the cancer removed and treated before making any decision about whether to have breast reconstruction.
Many women have a delayed reconstruction by choice, often some years after the original surgery. Unfortunately, in some areas of New Zealand women might experience a long wait to have this done in a public hospital. If you are considering having a delayed reconstruction and are no longer being seen for follow-up at the breast clinic, ask your GP to refer you to a plastic surgeon to discuss the options available to you.
Additional surgeries
With any breast reconstruction, additional surgical procedures may be required to achieve the best cosmetic outcome. Sometimes this might include fat grafting or surgery to the other breast, such as reduction of volume, or a breast lift procedure to achieve symmetry.
If you are having private treatment and have medical insurance, check your policy carefully and talk to your insurer. Many policies place a cap on the reimbursement amount and some don’t cover any surgery on the opposite breast.
What type of reconstruction is best for me?
Recent advances in reconstructive techniques give more choices for breast reconstruction. Each type of breast reconstruction has its own advantages and disadvantages and many factors are taken into consideration when deciding which method is most appropriate for an individual.
Factors to consider are:
- Your general state of health
- The amount of tissue available at potential donor sites
- The impact on your lifestyle and family responsibilities
- The likelihood of radiation therapy being needed
- The length and complexity of various procedures and recovery time
- The desired cosmetic outcome
- Patient and surgeon preference.
The surgeon will advise which procedures are suitable for you. All options may be suitable for some people, while others may have limited options. The choice then rests with you, as only you know which method will fit best with your lifestyle and expectations.
Depending on the type of surgery performed, recovery in hospital is usually between two to seven days requiring a further five to seven weeks to heal. In some cases it may be up to 12 weeks.
There are two main types of breast reconstruction:
- Implant reconstruction
- Autologous/autogenous reconstruction (using your own tissue)
Sometimes a combination of these two methods is used.
Scroll down for reconstruction diagrams and further explanations, and a video of New Zealand breast specialist surgeons sharing information on reconstruction techniques.
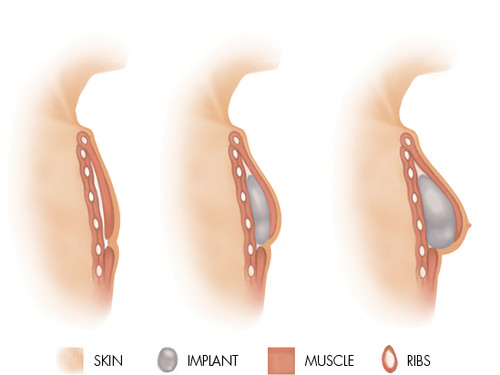
Implant reconstruction
This involves inserting a silicone breast implant underneath the skin and the muscle of the chest wall after the breast tissue has been removed. A tissue-expansion process is commonly needed first to create a cavity for the implant and gradually stretch the skin.
There are two implant reconstruction techniques used.
Two-stage procedure
A tissue expander is inserted at the time of mastectomy. This is a balloon-like device with a built-in fill port which can be easily located with a magnet and accessed with a needle via the skin. The expander is partially filled with saline (a salt solution) at the time of surgery.
Once the area has healed, more fluid is injected through the port over the course of several weeks to gradually increase the expander volume and stretch the muscle and skin. This creates a pocket big enough to hold a permanent implant which will match the size of the other breast.
The tissue-expander is often “over-expanded” to ultimately improve the shape of the reconstructed breast and provide a better match with the other side. Once filled, the expander is left in place for several months to let the skin adjust, before being replaced in a second operation, usually with a silicone gel implant. If any surgery is required to the other breast, for symmetry, it is done at this stage.
Implants used in breast reconstruction are usually made of a cohesive silicone gel (like an over-set jelly) which does not spill if the implant should rupture.
The outer shell of the implant is also made of silicone and has a textured surface, designed to reduce the risk of hardening around the implant (capsular contracture) and prevent the implant from rotating.
The implants are an anatomic or tear-drop shape to create a natural look.
Occasionally an implant with a distant, removable port may be used instead of a tissue expander. This type of implant has both a silicone and a saline component and can remain in place as a permanent implant once the desired volume has been reached and the separate port has been removed.
One-stage procedure
When sufficient skin has been preserved leaving an adequate envelope of skin and muscle to cover the implant, it may sometimes be possible to insert the definitive implant at the time of mastectomy.
The implant is placed under the pectoral muscle and is usually supported by a dermal matrix which supplements the strength and thickness of the mastectomy skin flaps and forms a supportive scaffolding to help hold the implant in place. This “mesh” is made of donated human or sometimes pig skin from which all cells have been removed. Over time it integrates into the surrounding tissue and becomes part of the structure of the reconstructed breast.
Implant reconstruction is often favoured for women who have smaller breasts and don’t want to have a long complex operation to take tissue from the abdomen, back or elsewhere.
Potential advantages of implant reconstruction:
- Shorter surgical procedure (although usually a two-stage operation)
- Shorter recovery time
- No donor site scars
Potential disadvantages:
- May need multiple appointments for tissue expansion
- The implant may eventually need replacement although modern implants have a very long life.
- Risk of capsular contracture. The body recognises the implant as a foreign body and forms a fibrous capsule around it to isolate it. In most cases this remains soft but in some cases it may harden and tighten and require removal.
- Less tolerance for radiation therapy. This can cause capsular contracture, skin thinning and breakdown and possible exposure of the implant. Tissue expansion may be limited in women who have had prior radiation therapy.
- A small risk of rupture or leakage. Modern implants are made of a cohesive gel which does not spill the implant contents if rupture occurs.
- Feels less natural and less mobile than a normal healthy breast.
- More difficult to match the other breast.
- Implant volume is fixed so will not continue to match the other side as the body ages or weight changes over time.
Although breast implants don’t increase the risk of breast cancer there is a very small risk of breast implant-associated anaplastic large cell lymphoma (a rare type of non-Hodgkins Lymphoma).
Most cases are cured by the removal of the implant and the surrounding capsule. It’s thought (but unproven) that chronic low-grade irritation from bacterial contamination of the implant may stimulate the immune system and cause cell transformation over time. The most common symptom of ALCL is a new swelling of the breast, caused by fluid accumulation. This usually develops between three and 14 years after implant placement.
There have been 10 known cases in New Zealand. Some of these had surgery performed overseas. For more information visit the New Zealand Association of Plastic Surgeons' website.
Autologous/autogenous reconstruction (reconstruction procedures that use your own tissue)
These procedures are complex and require a longer hospital stay and longer recovery time than implant reconstruction. There is significant scarring at the donor site and when muscle is used it may result in weakness at the donor site, but the use of natural tissue results in a breast that has a more natural look and feel.
Types of autologous flaps:
Flaps may be either pedicled or free.
Pedicled flaps
This method transfers skin, fat and muscle to the breast area on a pedicle or “stalk” of muscle which has not been fully detached from its original position and still contains the blood supply.
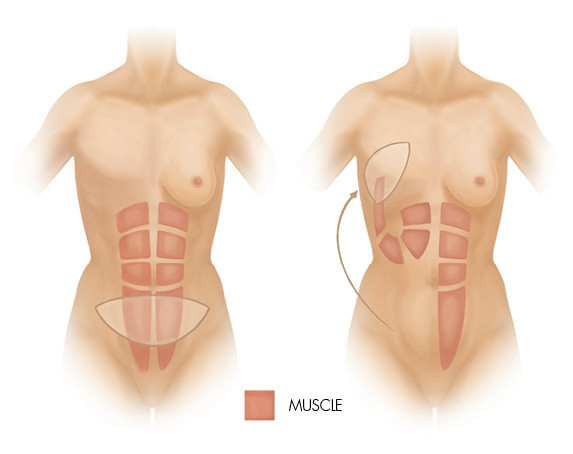
Pedicled TRAM flap reconstruction (Trans Rectus Abdominus Myocutaneous Flap)
In this surgery, a large abdominal incision is made from hip to hip at the bikini line. Skin, fat and part of the vertical “6-pack” muscle are transferred up to the breast by tunnelling under the abdomen. An area of abdominal skin fills in the defect on the central part of the breast and the other tissues create breast volume. The belly button is repositioned and the abdomen is flatter after removal of the tissue, resulting in a “tummy tuck”.
Recovery from this operation takes longer than implant surgery with a hospital stay of 5-7 days and a further 8-12 weeks of healing. There are restrictions on lifting, driving and major activity during the initial recovery period. This was once the most common autologous procedure but has largely been superseded by the DIEP flap.
Latissimus dorsi flap reconstruction
This operation is more suited to women with small to medium sized breasts and those who don’t wish to undergo TRAM or DIEP flap reconstruction.
It is often used for women who have:
- scarring from previous abdominal surgery
- abdominal tissue unsuited to the surgery. e.g. too thin or too large.
- a desire for future pregnancy
- previous failed abdominal flap or implant reconstruction.
It uses muscle (latissimus dorsi), fat and skin from the back. The flap, which remains partially attached so that it retains a blood supply, is transferred under the skin to the chest to form a breast mound. It usually doesn’t contain enough fat to give adequate breast volume so an implant is commonly used to supplement this.
The latissimus dorsi (lat. dorsi) is a large muscle that stabilises the shoulder joint and helps with reaching and twisting movements. Its removal from the back may reduce the ability to perform strenuous overhead activities with your arms. With physiotherapy most women have recovered most of their previous function one year after surgery. However, the procedure is generally not suited for active sportspeople.
Recovery from this operation involves a hospital stay of four to six days with a further recovery of six to eight weeks to allow for the wounds to heal and your body to adjust to the new location of the lat. dorsi muscle. You should avoid lifting or major physical activity for four weeks following the surgery.
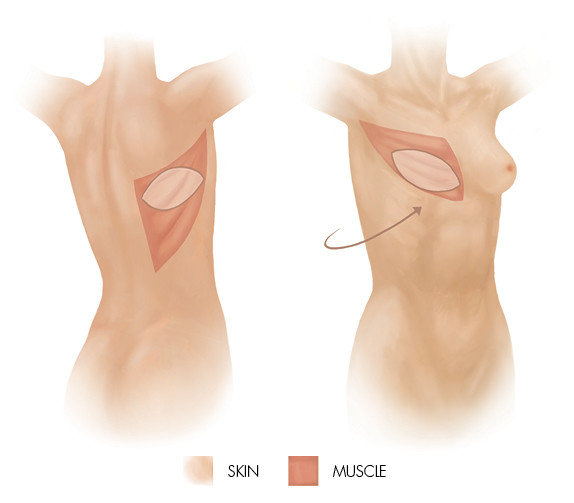
Extended latissimus dorsi flap
This method transfers more fat tissue than a standard lat. dorsi flap, to increase the volume of the reconstructed breast. It leaves a significant donor-site scar but avoids the need for an implant. There is a higher risk of seroma development, which usually settles after repeated aspirations, and some people experience muscle twitching if the nerve supply to the flap has been preserved. This can be corrected by severing the nerve.
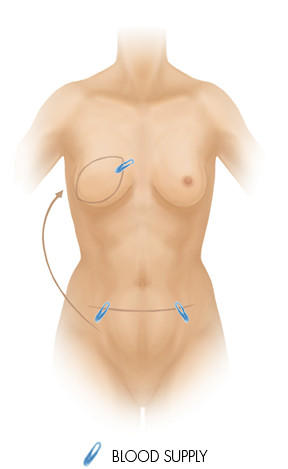
Free (microvascular) flaps
This method involves detaching skin, fat and some blood vessels completely from the donor site, and transferring them to the breast area where the blood supply is re-attached using microsurgery (the use of an operating microscope and small instruments).
DIEP Flap (Deep Inferior Epigastric artery Perforator)
The DIEP flap uses fat and skin from the same area of the abdomen as the TRAM flap, but doesn’t harvest the muscle to form the breast mound. This is a free flap, meaning the tissue is completely cut free from the donor site then transferred to the chest area. Microsurgery is used to connect the tiny blood vessels.
As the abdominal muscle is left intact, there is minimal loss of abdominal strength, generally less pain and a faster recovery compared with a pedicled TRAM flap.
Free TRAM flap
The free TRAM uses the same abdominal tissue as a pedicled TRAM (skin, fat, muscle) but the tissue is completely disconnected from the donor site and transferred to the chest where it is reconnected by microsurgery.
TUG (Transverse Upper Gracilis) flap
This procedure is used less commonly but may occasionally be used for women who are not suited to other autologous procedures and also don’t want implant reconstruction.
The TUG flap uses skin, fat and muscle from the upper thigh, near the groin, to reconstruct a breast. The scar is generally well hidden.
Gluteal flaps
This free flap procedure transfers tissue from the buttock to the chest area. It is rarely used but may be an option in limited circumstances.
Perforator flaps
The perforator flap is a more recent advance in microsurgery and can be used in appropriately selected women to repair defects in the breast after lumpectomy or partial mastectomy.
TDAP flap (ThoracoDorsal Artery Perforator)
A flap consisting of skin, fat and blood vessels is harvested from the same area on the back as the latissimus dorsi flap but avoids harvesting the muscle. The flap is rotated and tunnelled from the back onto the chest wall to fill the defect and create breast volume. The scar is usually well hidden along the bra line.
LiCAP flap (Lateral InterCostal Artery)
This uses redundant tissue from under the arm. There is a long scar on the side of the chest, going towards the back.
Potential advantages of autologous flaps:
- No implant needed (except latissimus dorsi flap)
- Results in a soft, natural looking breast
- Uses own tissue which changes with weight gain/loss and ageing
- More tolerant of radiation than implant reconstruction
Potential disadvantages of autologous flaps:
- Loss of strength due to muscle defect (except DIEP)
- Risk of hernia with abdominal flaps
- Large scar at donor site in addition to scar on the breast.
- More complex surgery and longer recovery time
- Seroma development (a collection of fluid which may sometimes require drainage)
- Risk of partial or complete flap failure.
Comparing reconstruction methods
It can be difficult to decide which reconstruction method will suit you best. Use this chart to compare methods.
| Implant | TRAM | DIEP | Latissimus Dorsi | |
| Implant Used? | Yes | No | No | May be used |
| Scarring | Breast only | Hip to hip at bikini line. Breast scar (usually circular in skin-sparing mastectomy) | Hip to hip at bikini line. Breast scar (usually circular in skin-sparing mastectomy) | Scar on back and breast |
| Muscle Effects | Little change | Weakened abdominal muscle | Little change | Slight weakness in shoulder or back |
| Breast Sensation | Little or no sensation | Little or no sensation | Little or no sensation | Little or no sensation |
| Operating Time | 3 hours | 4-6 hours | 6-8 hours | 6-7 hours |
| Hospital Stay | 2 days | 5-7 days | 5-7 days | 4-6 days |
| Recovery | 6-8 weeks | 6-12 weeks | 6-12 weeks | 6-12 weeks |
Other procedures
Fat grafting and lipofilling
Using liposuction, fat cells can be taken from other parts of the body (usually the abdomen, thighs or buttocks) and after processing to remove unwanted components they are injected in to the reconstructed breast to improve the contour, fill in defects or mask the outline of implants.
Over time, some of the fat will not be retained and repeat procedures may be required.
Nipple reconstruction
Once the reconstructed breast has healed and settled into position, a nipple can often be reconstructed surgically by raising flaps of tissue from the central area of the reconstruction. Over time the reconstructed nipple will likely undergo some degree of flattening. If women have large nipples, tissue can sometimes be grafted from one side to form a nipple on the other, resulting in smaller nipples on both sides.
Not all women choose to have a nipple reconstruction. Some may not feel the need to have a nipple to complete the look or may choose to use a prosthetic nipple, or have three-dimensional tattooing which creates the illusion of a raised nipple. Temporary 3D nipple “tattoos” are also available.
In reconstructed breasts with insufficient tissue, thin skin or radiation damage it may not be possible to perform nipple reconstruction.
Areola tattooing or micropigmentation
This final step in breast reconstruction gives colour to the nipple and creates the appearance of an areola around the nipple. Permanent colour pigments are blended to match your skin type and tattooed on to the skin under local anaesthetic. Several sessions may be needed to achieve the desired colour.
Oncoplastic surgery
Oncoplastic breast conservation surgery combines the disciplines of breast cancer surgery and plastic surgery to improve cosmetic outcomes without compromising the need to remove all of the cancer cells. Some breast surgeons in New Zealand have undergone further specialist training and are able to offer some of these procedures where appropriate. Others work with plastic surgeons for access to these techniques. This can enable some larger tumours to be excised without the need for mastectomy.
As with all breast conservation surgery for breast cancer, radiation therapy to the affected breast will still be required after these procedures. If the cancer has not been fully removed then further surgery will be required to achieve clearance. In some cases this may need to be a mastectomy.
Bilateral therapeutic mammoplasty
This combines breast conserving surgery with a breast reduction technique and can be used for appropriately selected women with large breasts and a tumour that may otherwise have required mastectomy. The lump can be removed with a wide rim of healthy tissue and the nipple areola complex is left intact. Reduction surgery is also performed on the other breast resulting in smaller, uplifted breasts. Radiation therapy will still be required for the affected breast.
Watch: Considering reconstruction after breast cancer
Visiting French surgeon Krishna Clough discussed different surgical options in his talk at the 2016 Australasian Breast Congress Consumer Day.
